This post is also available in Dutch .
Mental disorders are still growing worldwide, and for some, treatment remains ineffective. The diagnostic classification system of psychiatry (DSM) is often criticized. Is neuroscience the solution?
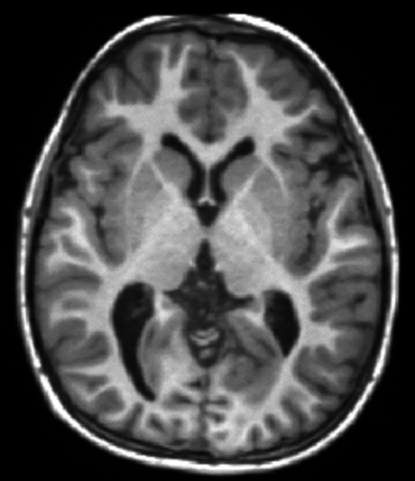
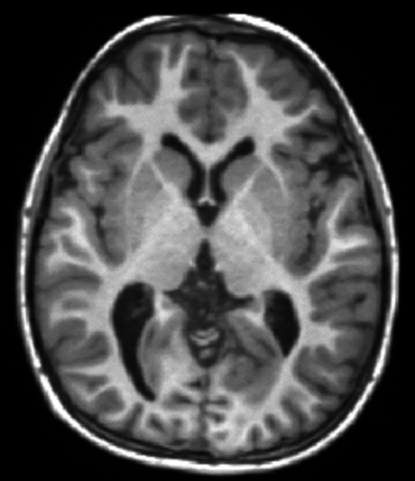
Image by Mim.cis – John Hopkins University, Public Domain, https://commons.wikimedia.org/w/index.php?curid=46493124. Image shows structural MRI scan of a human brain.
According to the World Health Organization, the burden of mental disorders continues to increase; it has social, economic, and health consequences worldwide. One of the central problems is our current diagnostic criteria and ineffective treatment. A diagnosis alone seems to be a poor predictor in choosing the right treatment. There are large individual differences in how people respond to treatment, where in some cases people do not benefit at all.
Problems with the current diagnostic tool of psychiatry
The diagnostic tools used in Psychiatry (DSM) right now are symptom-based: they rely on self-report of feelings and experiences by patients and on clinicians’ expertise and observations of behaviors. This subjective character of diagnostics has been shown to result in inconsistencies across patients and practitioners. Additionally, the diagnostic toolsare based on a classification system that looks at specific symptoms to classify individuals into distinct, non-overlapping categories. The problem here is that many disorders actually have overlapping symptoms and, to make things even more complicated, many patients who suffer from one disorder also have many traits of another, or even have multiple disorders at the same time! Thus, the boundaries between disorders are often not as strict as suggested by the DSM.
Mental disorders lie at the origin of the brain
Some see a solution to current diagnostic problems of the DSM by integrating more and more “objective” information into the DSM. One objective approach could be a brain scan that shows over- or under-active brain patterns that could be used to diagnose a mental disorder.
Mental disorders lie at the origin of the brain. Neuroscience, with its aims to understand normal and abnormal functioning of the human brain and mind (including cognition and emotions), is viewed as the study discipline that may be able to improve the more objective diagnostic criteria and treatment of mental disorders in the future.
TheUS National Institute of Mental Healthy (NIMH) proposed the Research Domain Criteria (RDoC)project in which 5 domains are central to psychopathology. The domains mainly focus on topics including emotion, cognition, motivation, and social behavior and each domain reflects a brain system in which functioning is impaired in different mental disorders. The RDoC is intended to facilitate the translation from neuroscience to clinical diagnosis and treatment. Importantly, the RDoC classifies mental disorders based on behavioural and neurobiological measures, e.g., a brain scan, that are less categorical in nature and not as prone to splitting up related disorders into separate boxes.
With this approach, we hope that risk factors as well as causes behind mental disorders can be better targeted to later improve treatment. Despite advances in neuroscience, there are still few to no steps incorporating neuroscience perspectives into the clinical setting. It will probably be a long-lasting endeavor which will include more educational and research efforts.
Written by Mahur. Edited by Annelies.